Fatty Liver Disease: Causes and Effective Treatment Options
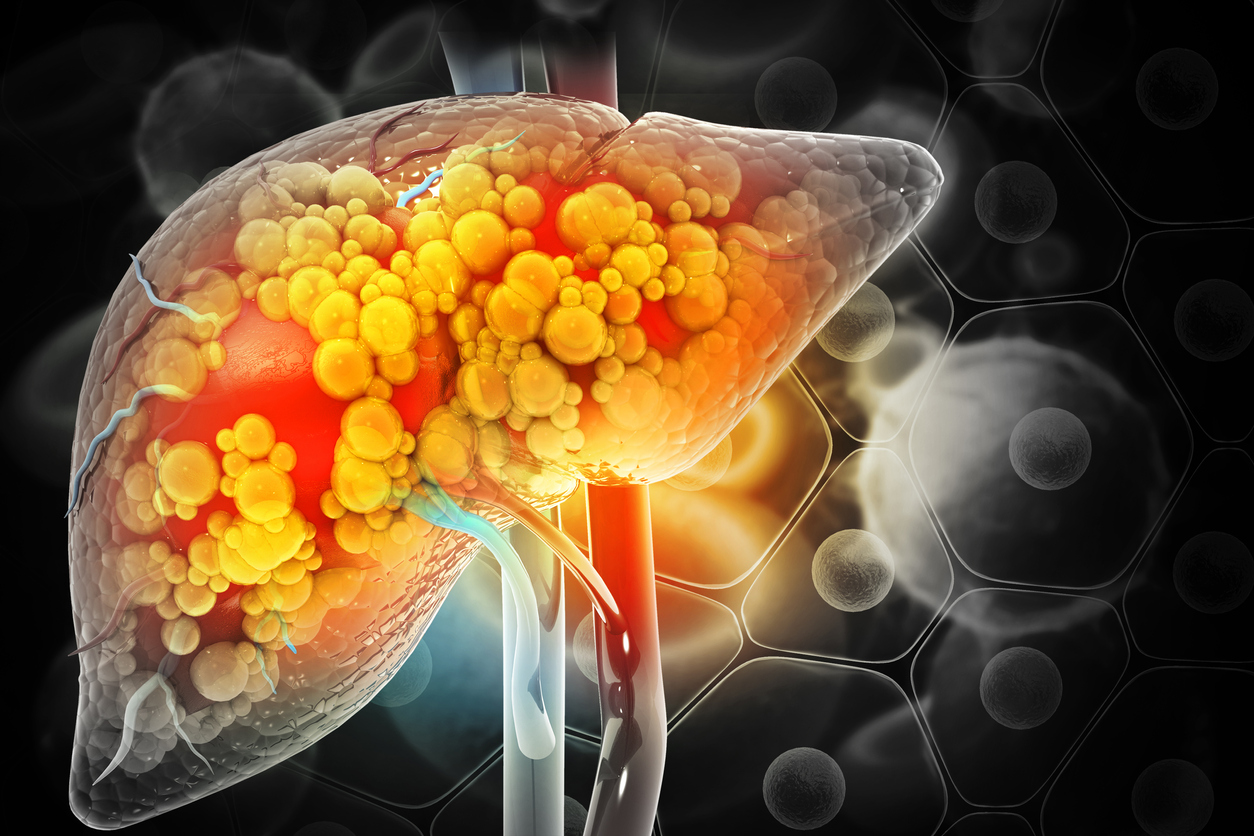
Introduction: Understanding Fatty Liver Disease
Fatty liver disease is a growing public health concern, affecting nearly one in three adults globally. It occurs when excess fat accumulates in the liver cells, impairing the liver’s ability to function correctly. The condition ranges from simple fat accumulation (steatosis) to inflammation and scarring, which can progress to more severe liver damage, including cirrhosis and liver failure.
Often linked to lifestyle and metabolic factors, fatty liver disease can develop silently, with few or no symptoms in its early stages. That’s why understanding its causes and pursuing appropriate treatment is crucial for preventing long-term complications and improving liver health.
What Is Fatty Liver Disease?
There are two primary types of fatty liver disease:
- Non-Alcoholic Fatty Liver Disease (NAFLD): This is the most common form and occurs in individuals who drink little to no alcohol. It’s closely tied to obesity, insulin resistance, and metabolic syndrome.
- Alcoholic Fatty Liver Disease (AFLD): This form results from excessive alcohol consumption, which directly harms liver cells and leads to fat accumulation and inflammation.
Regardless of the type, fatty liver disease can worsen over time if left untreated. In more advanced stages, the liver may develop fibrosis (scarring), cirrhosis, or even liver cancer.
What Causes Fatty Liver Disease?
The development of fatty liver disease is usually influenced by a combination of lifestyle, genetic, and metabolic factors.
Obesity and Overweight
Excess body fat, especially around the abdomen, is a significant risk factor. As body fat increases, so does the likelihood of fat accumulating in liver cells.
Insulin Resistance and Type 2 Diabetes
Insulin resistance leads to higher blood sugar levels, prompting the liver to produce more fat. Many individuals with fatty liver disease also have type 2 diabetes or prediabetes.
High Cholesterol and Triglycerides
Elevated levels of blood fats—especially triglycerides—are strongly associated with fatty liver development. These lipids are stored in the liver, resulting in fat accumulation over time.
Poor Diet
A diet high in saturated fats, added sugars, and refined carbohydrates could lead to fat accumulation in the liver. Foods like sugary drinks, processed snacks, fast food, and white bread are particularly harmful.
Sedentary Lifestyle
Lack of physical activity slows metabolism and contributes to weight gain, insulin resistance, and elevated blood fat levels, all of which are risk factors for fatty liver disease.
Excessive Alcohol Use
In alcoholic fatty liver disease, chronic alcohol consumption causes direct liver cell damage and triggers inflammation, fat accumulation, and eventual scarring.
Genetics and Family History
Some individuals have a genetic predisposition that makes them more susceptible to storing fat in the liver, even if they are not overweight or diabetic.
Symptoms of Fatty Liver Disease
Fatty liver disease often has no symptoms in the early stages, which makes routine screening important for those at risk. When symptoms do occur, they may include:
- Fatigue
- Discomfort or dull pain in the upper right abdomen
- Unexplained weight loss
- Weakness
- Elevated liver enzymes on blood tests
In advanced stages, symptoms may include jaundice (yellowing of the skin and eyes), fluid retention in the abdomen (ascites), and confusion due to toxins affecting the brain (hepatic encephalopathy).
Diagnosing Fatty Liver Disease
Diagnosis typically involves a combination of clinical evaluation, blood tests, imaging, and, in some cases, a liver biopsy.
- Blood tests: Liver enzymes (ALT, AST) may be elevated. Other blood work assesses glucose, cholesterol, and triglyceride levels.
- Imaging tests, such as ultrasound, CT scans, or MRI, can detect fat buildup in the liver.
- FibroScan: A specialized ultrasound that measures liver stiffness and fat content.
- Liver biopsy: In some cases, a sample of liver tissue is taken to assess inflammation and scarring.
Early detection is key to managing the disease before irreversible damage occurs.
Effective Treatment Options
The treatment for fatty liver disease primarily involves addressing the underlying causes. In most cases, lifestyle changes can significantly improve liver health and, in many instances, even reverse the buildup of fat.
Weight Loss
Losing 5–10% of total body weight has been shown to reduce liver fat, inflammation, and fibrosis. Gradual, sustainable weight loss achieved through a combination of diet and exercise is more effective and safer than crash dieting.
Improved Diet
Following a liver-friendly diet can halt the progression of fatty liver disease:
- Focus on vegetables, fruits, whole grains, legumes, and lean proteins.
- Choose healthy fats, such as those found in nuts, seeds, and olive oil.
- Avoid trans fats, processed foods, sugary beverages, and excessive red meat.
The Mediterranean diet is often recommended for individuals with fatty liver disease due to its anti-inflammatory benefits and balanced composition of healthy nutrients.
Regular Exercise
Engaging in at least 150 minutes of moderate aerobic activity per week can help reduce liver fat. Activities such as brisk walking, swimming, or cycling are particularly beneficial for maintaining good health.
Managing Blood Sugar and Cholesterol
Controlling diabetes and lowering cholesterol through medications or lifestyle changes is critical. Your healthcare provider may prescribe statins, metformin, or other agents, depending on your health profile.
Avoiding Alcohol
Even small amounts of alcohol can worsen liver damage, especially for those with existing fatty liver disease. Avoiding alcohol thoroughly is recommended for most individuals with the condition.
Medications Under Research
While there are no FDA-approved medications specifically for fatty liver disease yet, several treatments are in development. Some medicines used to treat diabetes and high cholesterol have shown promise in improving liver health.
Monitoring and Follow-Up
People diagnosed with fatty liver disease should work closely with their healthcare provider to monitor liver function and evaluate treatment progress. Regular blood tests, imaging studies, and lifestyle assessments are key to ensuring that the disease is being adequately managed.
Those with advanced liver disease may require care from a hepatologist (liver specialist) and additional treatments for complications such as cirrhosis or liver failure.
Potential Complications
If left untreated, fatty liver disease can lead to serious health problems:
- Liver fibrosis and cirrhosis: Scarring of liver tissue can impair function and lead to liver failure.
- Liver cancer: Individuals with advanced fibrosis or cirrhosis have a higher risk of developing hepatocellular carcinoma.
- Cardiovascular disease: Fatty liver is closely linked to heart disease and stroke.
- Kidney disease: Chronic liver conditions can also impact kidney function over time.
Conclusion: Taking Control of Liver Health
Fatty liver disease may be silent at first, but it has the potential to cause severe damage if ignored. Fortunately, with early intervention and sustained lifestyle changes, it is often reversible—especially in its early stages.
If you’re at risk or have been diagnosed, take proactive steps to improve your diet, lose excess weight, stay active, and avoid harmful substances like alcohol. Regular check-ups and liver monitoring will ensure that any complications are caught early.
Liver health is deeply connected to your overall well-being. By making wise, consistent choices, you can protect your liver and reduce the long-term risks associated with fatty liver disease.